In this article, we diurese the truth out of the many myths Lasix finds itself entangled in. The mystique is a consequence not of furosemide’s own fault, but of its ubiquity. We now understand many of the aphorisms surrounding frusi to be nothing more than folklore. The nephrologist’s ally and the cleaner’s nemesis, the number of applications for furosemide are only rivalled by the tricks up its sleeve. Forbid I run out of further words to alienate a dwindling audience and M’colleague catches on that this is a parody of his verbose writing, let us begin.
NOMENCLATURE – If your heart skips a beat to learn medical history
Malady: Nearly relegated to a dropdown box by an editor whose power grows with each passing day, this is the story of how furosemide came to be. And the spelling doesn’t matter. But it’s now furosemide. Deal with it.
Up til the early 1960s, the mainstay of diuresis was, quite confusingly, using mercury derivatives. The discovery that mercury containing compounds increase urine output was in itself a happy accident. One fine afternoon in 1919, Alfred Vogl – working in the Vienna clinic of the famous Wenckebach – identified diuresis as a peculiar side-effect of mercury-containing Novasurol (then a treatment for syphilis). Dr Vogl himself writes a charming account of this if you can look past the ethics of days past [1]. By no means was the diuretic effect interpreted by the great minds of the previous century that it is our body’s cry for help to dispose of a lethal toxin.
Thiazides were the first to come, and were later followed by a drug called Salu-58 in the German laboratory of Karl Sturm in 1959. The most potent diuretic then-identified [2]. Furosemide – a star was born. This variable nomenclature nonsense is merely a consequence of marketing, where it was known as furosemide in American markets and frusemide in the British. You may be interested to learn that since 2023, it is now christened FUROsemide in Australian markets too. As always, a reminder that “Lasix” is an amusing portmanteau derived from furosemide lasting six hours.
PHARMACOKINETICS – An Unhealthy Codependency with Albumin
Malady: Higher doses of furosemide are required in patients with moderate-severe hypoalbuminemia. Giving albumin with furosemide may not necessarily help.
A yearning for albumin is a box that many drugs tick. Very few are as invested as furosemide seems to be. The theory goes that when drugs bind to albumin, they are chauffeured around in a pharmacodynamically inert state of being, and the “free” unbound component is the clinically relevant effector. In furosemide’s case, it is a highly protein bound molecule (> 95%), but it also requires access to the luminal portion of the loops of Henle to be efficacious, a process that relies considerably on active secretion.
To boil down an hour spent obsessing over rat and rabbit studies – see two studies in 1987 [3] and in 1996 [4] – the changes induced by hypoalbuminemia are summarised as follows. Less furosemide is protein bound and distributes more widely (especially accumulating within the kidney). Without albumin, furosemide is metabolised and inactivated faster within the kidney. These studies suggest that the binding of albumin to furosemide facilitates its secretion into the proximal convoluted tubule and protects against being metabolised in the kidney, which in turn is essential for carrying out its function. As a result, even with moderate hypoalbuminemia, the efficacy of furosemide dips considerably with less diuresis and natriuresis observed. Ergo – higher doses of furosemide may be required in those with severe hypoalbuminemia.
Interestingly enough, I have seen this play out in a patient with severe nephrotic syndrome who required large doses of diuresis with their initial single digit albumin. With resolution of the hypoalbuminemia, the same doses became noticeably more potent.
So then is there a benefit to giving furosemide with an albumin chaser? Well, the evidence on this is mixed. There are some potential diuretic and natriuretic benefits purported by this meta-analysis [5], especially amongst those who are more severely malnourished and with higher doses of albumin, but the clinical question of does this lead to meaningful changes in fluid status is not yet answered. I suspect giving a diuretic with a colloid (albumin) that will only hold on to further fluid is not borne from the brightest tool in the shed.
PHARMACODYNAMICS – A Culprit for Hyponatremia? Think Again.
Malady: Despite directly blocking sodium reabsorption, furosemide does not cause hyponatremia in isolation.
Like thiazides and mineralocorticoid receptor antagonists, furosemide interferes with the reabsorption of solute from the glomerular filtrate. Hyponatremia is often a dose limiting side effect of these cousin diuretics, particularly in the case of thiazides. Despite the many instances of suspended furosemides in hyponatremic patients you would have encountered, it was likely nothing more than a bystander to the madness.

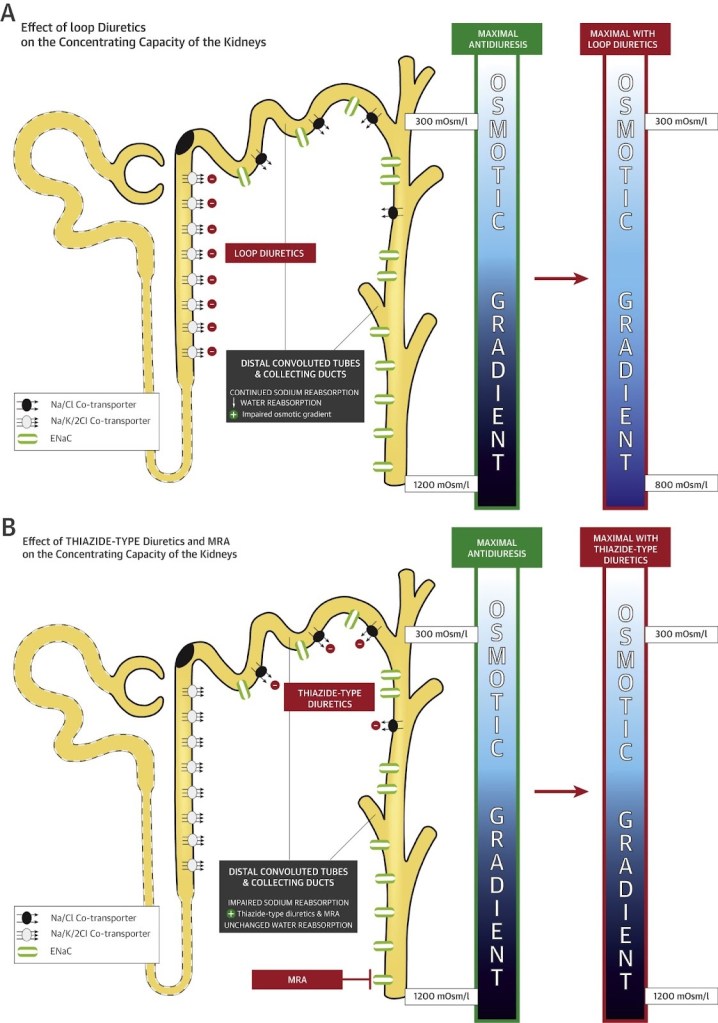
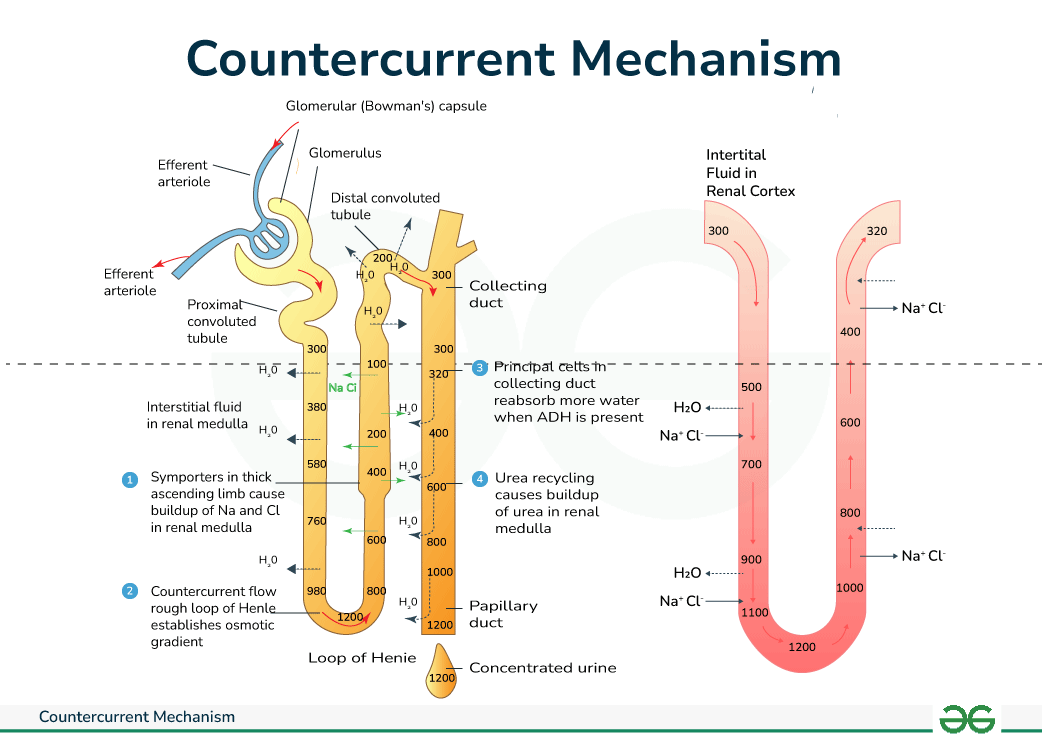
First, a trip back to medical school. Hidden amongst the labyrinth of reabsorption channels in the latter half of the nephron is the mighty countercurrent multiplier (see Figure 1). In the water-impermeable ascending loop of Henle, active transport of ions from the filtrate into the medullary interstitium creates a very hypertonic (solute >> water) environment. This process is largely dependent on the Na-K-2Cl channel. This is leveraged in the descending loop of Henle and the collecting duct where water is drawn from the relatively hypotonic (water > solute) filtrate back into the circulation, using this concentration gradient generated in the renal medulla. This is how the bulk of water that filters through the glomeruli is re-absorbed, with the Na/Cl channel (thiazide target), aldosterone (spironolactone target) and ADH/vasopressin also helping to modulate the extent.
Through its action on the Na-K-2Cl transporter in the ascending loop of Henle, furosemide disrupts the buildup of high interstitial osmolality in the renal medulla (see Figure 2) to narrow the concentration gradient across which the kidney can reabsorb water. Since the reabsorption is still through a concentration gradient, the ratio of Na-to-free water excreted is more equitable in the case of loop diuretics when compared to MRAs and thiazides. The urine produced in response to loop diuretics has a lower Na concentration (less natriuresis, more diuresis) than their thiazide and MRA cousins [6]. In fact, this goes as far as furosemide being a treatment for hyponatremia [7] – but note that this protective effect does not necessarily apply to patients already on other diuretics.
CLINICAL UTILITY – Furosemide in Acute Pulmonary Oedema. Not All that Glimmers is Golden (Urine).
Malady: Furosemide’s benefit in APO is not solely diuresis-related. It is a potent venodilator that is responsible for its initial efficacy before the diuretic effect later takes over.
Surprisingly, this misconception begins at genesis. Nearly half of patients presenting with decompensated heart failure do not exhibit preceding weight gain of over 0.9kg – in essence, hypervolemia is not a necessary feature of many patients with APO [8].
We know that furosemide’s effect in APO must not be limited to just diuresis since many patients notice near-immediate symptomatic relief, prior to a spike in urinary output being achieved. Furosemide actually has additional direct vascular effects responsible for its initial and immediate efficacy. A landmark 1973 investigation in NEJM [9] neatly outlines that while it takes 30-60 minutes for urine flow and natriuresis respectively, there is a near-immediate drop in left ventricular filling pressure (suggestive of reduced preload) suspected to be due to an increase in venous capacitance from venodilation.
As an aside, this same mechanism likely underlies the use of furosemide in equine exercise-induced pulmonary haemorrhage – a phenomenon of epistaxis and haemorrhage where horses and greyhounds are stressed well beyond physiological limits resulting in high pulmonary pressures that fracture maladapted capillaries [9]. This use of furosemide serves as a reflection of how human ingenuity can and will unfortunately overcome human morality.
To the clever cookies now eager to dispense furosemide to venodilate anuric patients, I fear that a more recent investigation of this failed to find a clinically meaningful haemodynamic change, but it did not specifically investigate those with pulmonary oedema [10]. To offset your disappointment, I offer an olive branch in return – in those with minimal urine output in response to diuresis, consider a urine sodium a few hours after treatment is initiated to clarify the amount of natriuresis (i.e. diuretic response). This helps to avoid dosing beyond the ceiling, where toxicity is encountered for little payoff.
FIN
For a drug we use very frequently, furosemide has many quirks that should modify our utilisation of it. The reliance on outdated studies and a lack of subsequent investigations in humans to establish key properties of a ubiquitous medication is puzzling to say the least. There are more myths that lace the contradictorily termed water pill, which we can cover in another part if this was not satisfactorily tedious.
Giant’s Shoulders:
[1] Vogl and mercury-based diuresis
[2] A (absolutely not) brief history of diuretics
Furosemide and Protein – study in rodents [3] and in rabbits [4]
[9] The 1973 study about furosemide’s additional effects in pulmonary oedema
Also Cited Above:
[5] Meta-analysis by Lee and colleagues re: albumin co-administration with furosemide
[6] Hyponatremia and diuretics – a detailed review
[7] Lapsia and Kazory (2010) on using loop diuretics as a therapeutic option for hyponatremia
[8] Chaudhry et al (2010) – tracking weight gain around times of heart failure related hospitalisations
[9] MSD Vet Manual about fractured horse capillaries 😦
[10] Detailed investigation of cardiovascular effects of furosemide in anuric haemodialysis patients by Hayashi et al (2008)
Discover more from Myths & Maladies
Subscribe to get the latest posts sent to your email.
1 Comment
Comments are closed.