Myth: Thyroid ultrasounds comprise the standard work-up for abnormal TFTs
Malady: Think twice before ordering a thyroid ultrasound. They’re probably gonna cause more grief than diagnostic benefit.
I’m a very lucky man. Not because of the hundreds of loyal fans who stop me on the street and ask for a selfie. Honestly, who knew an outlet for anger management masquerading as a medical blog could get you reservations at the best restaurants. Zouki’s, Jamaica Blue – you name it, they want me there.
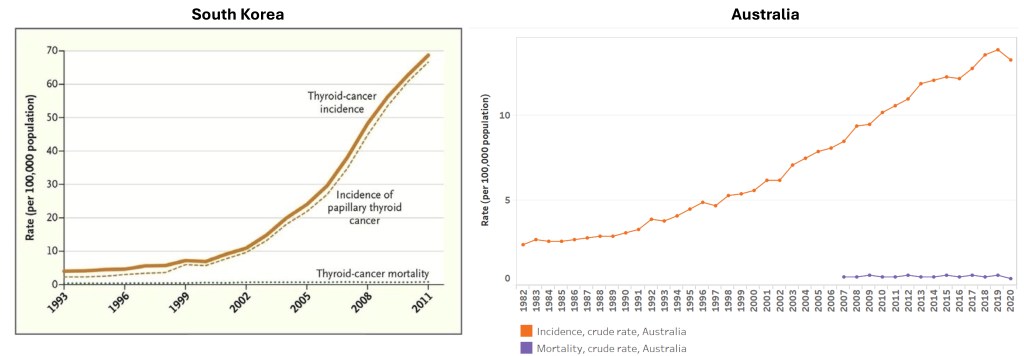
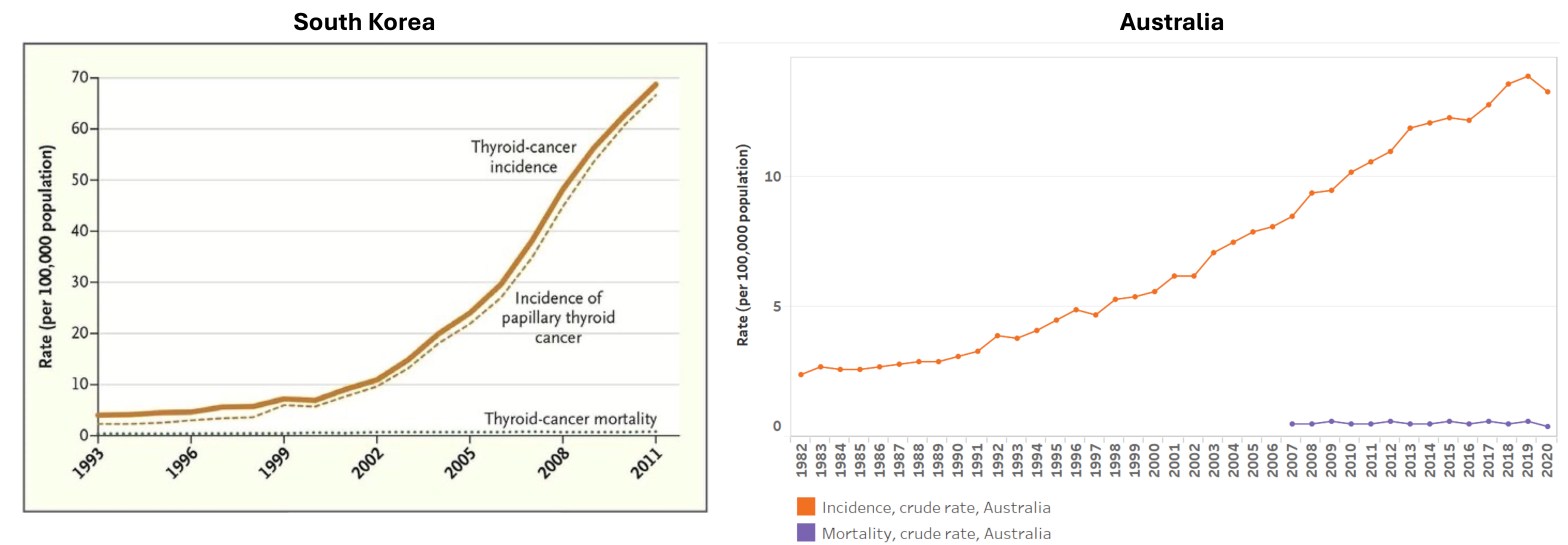
Putting aside my valiant efforts to cancel us, I recently found out that I practice and serve in a community which undergoes the highest number of thyroid ultrasounds in Australia [1]. Technically Canberra East is the highest, but no one lives there so their standardised rate doesn’t count. Before you blame the thoroughness of my South West Sydney kin, this is in fact a global pandemic among high-income countries. Aside from a few places like New Zealand, Denmark, Norway (aka countries which somehow consistently do things right it makes me suspicious), and the UK (aka countries whose health system are crumbling), we seem to love imaging the thyroid (Figure 1). Probably because most of us can’t tell the difference between neck fat and glandular tissue on palpation – I have calluses from playing the guitar, what’s your excuse?

The biggest proponents in this game are South Korea, who have a National Screening program for every screenable cancer basically in turn for a small co-payment (of course), and it is here I’ve collected the receipts to back my turf war with privately-owned radiology practices.
Everyone has a Nodule, and No One’s Dead
Thyroid nodules are basically skin tags of the neck. Up to 65% of the population has one discovered incidentally during imaging [3]. It seems rates vary, but around 10% of thyroid nodules are in turn thyroid cancers. And, 85% of these cancers are papillary, and 12% follicular – both terrifying names for tumours that are much less threatening than one of those bug-eyed Labubus I saw dangling off an intern’s backpack last week (look it up it’s a thing [4 – reference for their abysmal mortality rate, not the Labubu]. Figure 2 is a testament to how good we have become not at curing thyroid cancer but at detecting it. Both in South Korea and here in Australia, incidence of thyroid cancer has exponentially increased, while mortality rates have remained the same, that is, still very low.
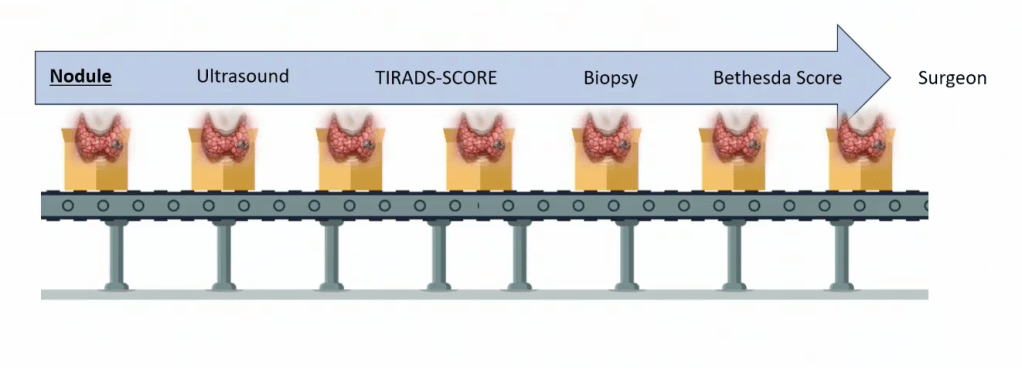
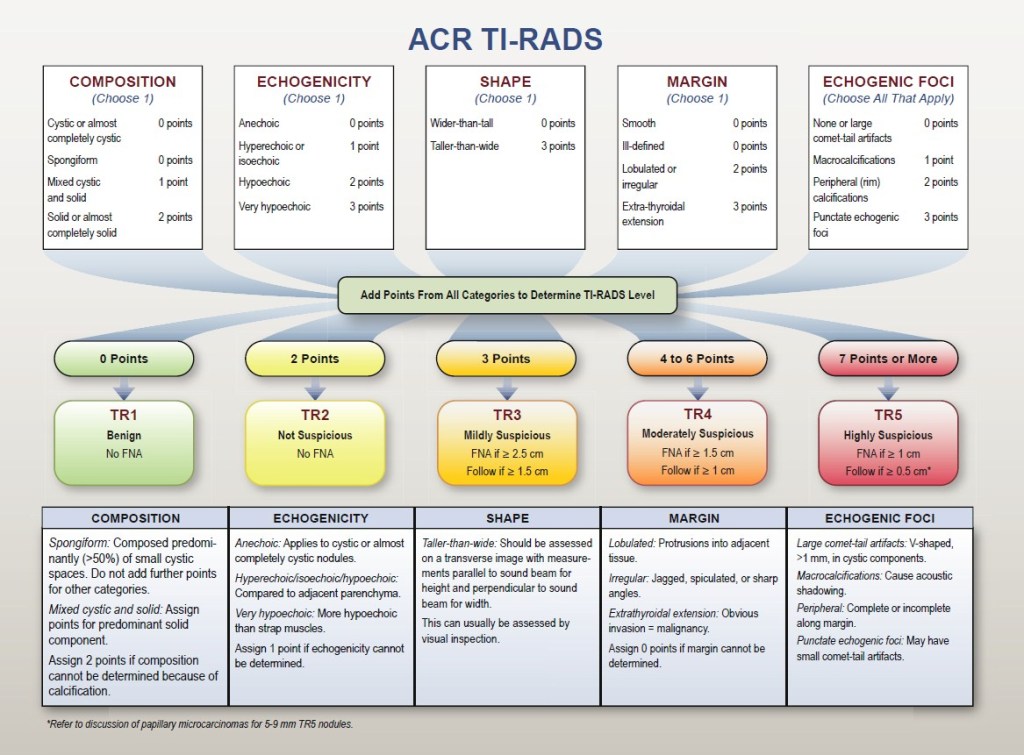
Dr Christopher Rowe in his 2025 Endocrinology Society of Australia Seminar (name drop) describes a conveyor belt not unlike our lives in medicine (Figure 3). Incidentaloma is found on CT. Ultrasound is performed, and everything in the face of the Earth is given a TI-RADS* score whether it’s a real nodule or not. Now they undergo surveillance with repeat ultrasound until the private radiology practice grows a conscience faster than the patient grows a non-existent tumour, or get biopsies which show nothing.
So what should we do?
Guidelines actually exist (who knew)
Don’t let FOMO guide your decision-making. The TSH Tsars, the High Priests of Hormones and the Gatekeepers of Glucose recommend:
- DO NOT order a thyroid ultrasound as part of hyperthyroidism or hypothyroidism work-up. If someone’s got the bloods and no palpable lump, then ultrasound adds as much value as a GCS on a toe. This goes to say, hands to necks please – examine your patient.
- DO NOT chase every incidentaloma. That 8 mm nodule the Radiologist described because they ran out of things to say about the brain? It’s fine. Let it free. Learn a few things from the upstanding mostly men of the Southern District of New York. Order some TFTs. Find that copy of Talley’s from med school and perform a thyroid exam. If there are palpable nodules, go to point 6.
- DO NOT apply TI-RADS to things that are not nodules (duh). This includes a diffuse increase in the size of the thyroid, and confluent nodularity.
- DO NOT biopsy functional nodules (endocrinologists call them hot, but tbh I don’t really see it). Toxic adenoma or toxic nodular goitre are just that. They’re usually not cancer [7, 8]. Okay I get it there is an element of uncertainty you poorly-adjusted human beings aren’t comfortable with. But the point is that thyroid cancer is the most forgiving of the cancers – we have the time and scope to allow for much more uncertainty.
- This is for the nerds out there, but DO NOT apply TI-RADS to nodules after radioactive iodine – they become solid, hypo echoic and calcified over time – automatically TR4+ [9, 10]
- DO order an ultrasound in the initial work-up of a palpable thyroid nodule. If it really is a nodule, then you can go down the conveyor belt and get to use cool words like Bethesda and
samosapsammoma. - DO be concerned about rapidly growing thyroid nodules. This should herald suspicion for poorly-differentiated or medullary carcinoma.
You may sometimes find a FDG-PET avid thyroid nodule in your quest to look for some other devastating cancer. FDG avidity may be due to an overactive nodule, inflammation (even immunotherapy can cause this), or in 30-40% of cases, thyroid cancer [11, 12]. So the recommendation is to ultrasound these and possibly biopsy them, but usually only after the primary cancer is sorted.
So, bottom line – I advocate for reduced cancer surveillance to improve the quality of life of my patients. Next up, adrenal adenomas.
* For those not cool enough to think about T3 and T4 all day, TI-RADS is a scoring system (out of 14 but it gets distilled into 5 stages because that makes sense) to determine which nodules are suspicious enough to biopsy. It provides guidance based on ultrasound features and size on which nodules should be investigated further with an FNA.
Giant’s Shoulders
I credit my good friend and Professor Emeritus of Verbal Innovation, Dr Khan who made the recommendation for this topic, during what could only be described as a TED Talk with no audience.
Also cited above
[1] Australian Commission on Safety and Quality in Healthcare. Australian Atlas of Healthcare Variation (2017 data). https://www.safetyandquality.gov.au/our-work/healthcare-variation/third-atlas-2018/atlas-2018-3-thyroid-investigations-and-treatments/32-neck-ultrasound-and-thyroidectomy-18-years-and-over
[2] Li M, Maso LD, Vaccarella S. Global trends in thyroid cancer incidence and the impact of overdiagnosis. The Lancet Diabetes & Endocrinology. 2020;8(6):468-70.
[3] Radiopaedia. Incidental thyroid nodule. 2025. https://radiopaedia.org/articles/incidental-thyroid-nodule-1
[4] Wong R, Farrell SG, Grossmann M. Thyroid nodules: diagnosis and management. Med J Aust. 2018;209(2):92-8.
[5] Ahn Hyeong S, Kim Hyun J, Welch HG. Korea’s Thyroid-Cancer “Epidemic” — Screening and Overdiagnosis. New England Journal of Medicine.371(19):1765-7.
[6] Australian Institute of Health and Welfare. Cancer data in Australia. https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia/contents/state-and-territory
[7] Mon SY, Riedlinger G, Abbott CE, Seethala R, Ohori NP, Nikiforova MN, et al. Cancer risk and clinicopathological characteristics of thyroid nodules harboring thyroid-stimulating hormone receptor gene mutations. Diagn Cytopathol. 2018;46(5):369-77.
[8] Lau LW, Ghaznavi S, Frolkis AD, Stephenson A, Robertson HL, Rabi DM, Paschke R. Malignancy risk of hyperfunctioning thyroid nodules compared with non-toxic nodules: systematic review and a meta-analysis. Thyroid Res. 2021;14(1):3.
[9] Croker EE, McGrath SA, Rowe CW. Benign Thyrotoxic Nodules Become Solid, Hypoechoic, and Calcified on Ultrasonography Following Radioiodine Administration. Clinical Thyroidology®. 2023;35(6):232-5.
[10] Koç I, Bahçecioğlu AB, Avcı Merdin F, Araz M, Erdoğan MF. Long-term effects of radioiodine treatment on thyroid functions and ultrasonographic features in patients with toxic adenoma and toxic multinodular goitre. Ann Nucl Med. 2023;37(6):371-9.
[11] Pattison DA, Bozin M, Gorelik A, Hofman MS, Hicks RJ, Skandarajah A. (18)F-FDG-Avid Thyroid Incidentalomas: The Importance of Contextual Interpretation. J Nucl Med. 2018;59(5):749-55.
[12] Wadsley J, Balasubramanian SP, Madani G, Munday J, Roques T, Rowe CW, et al. Consensus statement on the management of incidentally discovered FDG avid thyroid nodules in patients being investigated for other cancers. Clin Endocrinol (Oxf). 2024;101(5):557-61.
[13] Tessler FN, Middleton WD, Grant EG, Hoang JK, Berland LL, Teefey SA, et al. ACR Thyroid Imaging, Reporting and Data System (TI-RADS): White Paper of the ACR TI-RADS Committee. J Am Coll Radiol. 2017;14(5):587-95.
Discover more from Myths & Maladies
Subscribe to get the latest posts sent to your email.
1 Comment
Comments are closed.